Abstract
Research Article
Factors Associated with Elevated Transcranial Doppler Ultrasound Velocities in Children With Sickle Cell Anemia in Mwanza, Tanzania
Georgina George Balyorugulu, Emmanuela Ambrose, Patrick S Ngoya, Yusuf S Jamnagerwalla, Iddi S Buri, Primrose Songoro and Protas D Komba
Published: 28 July, 2023 | Volume 6 - Issue 2 | Pages: 033-038
Background: Stroke occurs in 11% of patients with SCA before 20 years of age. In Northwestern Tanzania, the prevalence of stroke among children living with SCA under the age 15 years is 16.9%, of which might be attributed to the absence of routine screening for the risk of stroke by using Transcranial Doppler Ultrasound (TCD). Screening with TCD allows preventive measures such as chronic blood transfusion to be done which has led to the reduction of stroke by 92%.
Methods: This was a prospective analytical cross sectional study which enrolled 267 SCA children aged 2 to 16 years attending Bugando Medical Centre Pediatric Sickle Cell Clinic from July 2019 to June 2020. Assessment of factors associated with elevated TCD included a clinical history of stroke in sibling, death in sibling, temperature, oxygen saturation in room air, blood pressure, hemoglobin level and total white blood cell count. TCD was done by accessing transtemporal window and recording the highest time average mean of maximum velocity (TAMMV) of major vessels mainly, middle cerebral artery (MCA) and distal internal carotid artery (dICA).
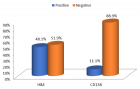
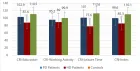
Results: The median age of enrolled was 6.6 (IQR: 4-9) years. The prevalence of elevated TCD (> 170 cm/s)
was found to be 21% (56/267). By multivariate logistic regression, low oxygen saturation in room air, p - value = 0.037, OR 1.08 [95% CI 1.00-1.17] and low hemoglobin level, p - value = 0.001, OR 1.76 [95% CI 1.26-2.45] were statistically significantly associated with elevated TCD among children living with SCA.
Conclusion: The high prevalence of elevated TCD velocity, with low hemoglobin and low oxygen saturation in room air as associated factors under multivariate logistic regression, warrants routine TCD screening for children with SCA aged 2 to 16 years.
Read Full Article HTML DOI: 10.29328/journal.japch.1001058 Cite this Article Read Full Article PDF
References
- Ilesanmi OO. Pathological basis of symptoms and crises in sickle cell disorder: implications for counseling and psychotherapy. Hematol Rep. 2010 Jan 26;2(1):e2. doi: 10.4081/hr.2010.e2. Epub 2010 Apr 13. PMID: 22184515; PMCID: PMC3222266.
- Minneci PC, Deans KJ, Zhi H, Yuen PS, Star RA, Banks SM, Schechter AN, Natanson C, Gladwin MT, Solomon SB. Hemolysis-associated endothelial dysfunction mediated by accelerated NO inactivation by decompartmentalized oxyhemoglobin. J Clin Invest. 2005 Dec;115(12):3409-17. doi: 10.1172/JCI25040. Epub 2005 Nov 17. PMID: 16294219; PMCID: PMC1283939.
- Switzer JA, Hess DC, Nichols FT, Adams RJ. Pathophysiology and treatment of stroke in sickle-cell disease: present and future. Lancet Neurol. 2006 Jun;5(6):501-12. doi: 10.1016/S1474-4422(06)70469-0. PMID: 16713922.
- Be smart, Know about Sickle Cell Disease! https://afro.who.int/news/be-smart-know-about-sickle-cell-disease.
- Ambrose EE, Makani J, Chami N, Masoza T, Kabyemera R, Peck RN, Kamugisha E, Manjurano A, Kayange N, Smart LR. High birth prevalence of sickle cell disease in Northwestern Tanzania. Pediatr Blood Cancer. 2018 Jan;65(1):10.1002/pbc.26735. doi: 10.1002/pbc.26735. Epub 2017 Aug 2. PMID: 28766840; PMCID: PMC5701733.
- Ambrose EE SL, Charles M, Hernandez AG, Latham T, Hokororo A, Beyanga M, Tebuka E, Howard TA, Ware RE. Geospatial mapping of sickle cell disease in Northwestern Tanzania: The Tanzanian Sickle Surveillance Study (TS3). Blood. 2018 Nov;132 (Suppl 1):3662.
- Saidi H, Smart LR, Kamugisha E, Ambrose EE, Soka D, Peck RN, Makani J. Complications of sickle cell anaemia in children in Northwestern Tanzania. Hematology. 2016 May;21(4):248-256. doi: 10.1080/10245332.2015.1101976. Epub 2016 Feb 17. PMID: 26868490; PMCID: PMC4972452.
- Adams RJ, Nichols FT, Figueroa R, McKie V, Lott T. Transcranial Doppler correlation with cerebral angiography in sickle cell disease. Stroke. 1992 Aug;23(8):1073-7. doi: 10.1161/01.str.23.8.1073. PMID: 1636180.
- Makani J, Kirkham FJ, Komba A, Ajala-Agbo T, Otieno G, Fegan G, Williams TN, Marsh K, Newton CR. Risk factors for high cerebral blood flow velocity and death in Kenyan children with Sickle Cell Anaemia: role of haemoglobin oxygen saturation and febrile illness. Br J Haematol. 2009 May;145(4):529-32. doi: 10.1111/j.1365-2141.2009.07660.x. Epub 2009 Mar 27. PMID: 19344425; PMCID: PMC3001030.
- tawananet.or.tz.
- Sub-Divisional Population Projection for year 2016 and 2017 Based on 2012 population and housing census. National Bureau of statistics.
- https://www.bugandomedicalcentre.go.tz/.
- Ohene-Frempong K, Weiner SJ, Sleeper LA, Miller ST, Embury S, Moohr JW, Wethers DL, Pegelow CH, Gill FM. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998 Jan 1;91(1):288-94. PMID: 9414296.
- Adams RJ, McKie VC, Brambilla D, Carl E, Gallagher D, Nichols FT, Roach S, Abboud M, Berman B, Driscoll C, Files B, Hsu L, Hurlet A, Miller S, Olivieri N, Pegelow C, Scher C, Vichinsky E, Wang W, Woods G, Kutlar A, Wright E, Hagner S, Tighe F, Waclawiw MA, et al. Stroke prevention trial in sickle cell anemia. Control Clin Trials. 1998 Feb;19(1):110-29. doi: 10.1016/s0197-2456(97)00099-8. PMID: 9492971.
- Alexandrov AV, Sloan MA, Tegeler CH, Newell DN, Lumsden A, Garami Z, Levy CR, Wong LK, Douville C, Kaps M, Tsivgoulis G; American Society of Neuroimaging Practice Guidelines Committee. Practice standards for transcranial Doppler (TCD) ultrasound. Part II. Clinical indications and expected outcomes. J Neuroimaging. 2012 Jul;22(3):215-24. doi: 10.1111/j.1552-6569.2010.00523.x. Epub 2010 Oct 26. PMID: 20977531.
- Adams RJ, McKie VC, Carl EM, Nichols FT, Perry R, Brock K, McKie K, Figueroa R, Litaker M, Weiner S, Brambilla D. Long-term stroke risk in children with sickle cell disease screened with transcranial Doppler. Ann Neurol. 1997 Nov;42(5):699-704. doi: 10.1002/ana.410420505. PMID: 9392568.
- Hoppe C. Defining stroke risk in children with sickle cell anaemia. Br J Haematol. 2005 Mar;128(6):751-66. doi: 10.1111/j.1365-2141.2004.05310.x. PMID: 15755278.
- Adams RJ, McKie VC, Hsu L, Files B, Vichinsky E, Pegelow C, Abboud M, Gallagher D, Kutlar A, Nichols FT, Bonds DR, Brambilla D. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med. 1998 Jul 2;339(1):5-11. doi: 10.1056/NEJM199807023390102. PMID: 9647873.
- Kuboyama T, Hori A, Sato T, Mikami T, Yamaki T, Ueda S. Changes in cerebral blood flow velocity in healthy young men during overnight sleep and while awake. Electroencephalogr Clin Neurophysiol. 1997 Feb;102(2):125-31. doi: 10.1016/s0921-884x(96)95054-7. PMID: 9060863.
- Bernaudin F, Verlhac S, Chevret S, Torres M, Coic L, Arnaud C, Kamdem A, Hau I, Grazia Neonato M, Delacourt C. G6PD deficiency, absence of alpha-thalassemia, and hemolytic rate at baseline are significant independent risk factors for abnormally high cerebral velocities in patients with sickle cell anemia. Blood. 2008 Nov 15;112(10):4314-7. doi: 10.1182/blood-2008-03-143891. Epub 2008 Sep 4. Erratum in: Blood. 2010 Dec 2;116(23):5079. PMID: 18772456.
- Powars D, Hiti A. Sickle cell anemia. Beta s gene cluster haplotypes as genetic markers for severe disease expression. Am J Dis Child. 1993 Nov;147(11):1197-202. doi: 10.1001/archpedi.1993.02160350071011. PMID: 8237915.
- Dorie A, Guindo A, Saro YS, Toure BA, Fane B, Dembele AK, et al. [Screening of cerebral vasculopathy in sickle cell anemia children using transcranial Doppler]. Arch Pediatr. 2015 Mar;22(3):260-6.
- Lagunju I, Sodeinde O, Telfer P. Prevalence of transcranial Doppler abnormalities in Nigerian children with sickle cell disease. Am J Hematol. 2012 May;87(5):544-7. doi: 10.1002/ajh.23152. Epub 2012 Mar 28. PMID: 22460323.
- Lagunju I, Sodeinde O, Brown B, Akinbami F, Adedokun B. Transcranial Doppler ultrasonography in children with sickle cell anemia: Clinical and laboratory correlates for elevated blood flow velocities. J Clin Ultrasound. 2014 Feb;42(2):89-95. doi: 10.1002/jcu.22099. Epub 2013 Oct 26. PMID: 24166013.
- Leite AC, de Oliveira RV, de Moura PG, Silva CM, Lobo C. Abnormal transcranial Döppler ultrasonography in children with sickle cell disease. Rev Bras Hematol Hemoter. 2012;34(4):307-10. doi: 10.5581/1516-8484.20120078. PMID: 23049447; PMCID: PMC3460401.
- Silva CM, Giovani P, Viana MB. High reticulocyte count is an independent risk factor for cerebrovascular disease in children with sickle cell anemia. Pediatr Blood Cancer. 2011 Jan;56(1):116-21. doi: 10.1002/pbc.22680. Epub 2010 Oct 14. PMID: 20949593.
- Bernaudin F, Verlhac S, Arnaud C, Kamdem A, Chevret S, Hau I, Coïc L, Leveillé E, Lemarchand E, Lesprit E, Abadie I, Medejel N, Madhi F, Lemerle S, Biscardi S, Bardakdjian J, Galactéros F, Torres M, Kuentz M, Ferry C, Socié G, Reinert P, Delacourt C. Impact of early transcranial Doppler screening and intensive therapy on cerebral vasculopathy outcome in a newborn sickle cell anemia cohort. Blood. 2011 Jan 27;117(4):1130-40; quiz 1436. doi: 10.1182/blood-2010-06-293514. Epub 2010 Nov 10. PMID: 21068435.
- Cox SE, Makani J, Soka D, L'Esperence VS, Kija E, Dominguez-Salas P, Newton CR, Birch AA, Prentice AM, Kirkham FJ. Haptoglobin, alpha-thalassaemia and glucose-6-phosphate dehydrogenase polymorphisms and risk of abnormal transcranial Doppler among patients with sickle cell anaemia in Tanzania. Br J Haematol. 2014 Jun;165(5):699-706. doi: 10.1111/bjh.12791. Epub 2014 Feb 21. PMID: 24666344; PMCID: PMC4154124.
- Quinn CT, Sargent JW. Daytime steady-state haemoglobin desaturation is a risk factor for overt stroke in children with sickle cell anaemia. Br J Haematol. 2008 Feb;140(3):336-9. doi: 10.1111/j.1365-2141.2007.06927.x. Epub 2007 Nov 27. PMID: 18042265; PMCID: PMC2562641.
- Dutra FF, Alves LS, Rodrigues D, Fernandez PL, de Oliveira RB, Golenbock DT, Zamboni DS, Bozza MT. Hemolysis-induced lethality involves inflammasome activation by heme. Proc Natl Acad Sci U S A. 2014 Sep 30;111(39):E4110-8. doi: 10.1073/pnas.1405023111. Epub 2014 Sep 15. PMID: 25225402; PMCID: PMC4191786.
- Gladwin MT, Ofori-Acquah SF. Erythroid DAMPs drive inflammation in SCD. Blood. 2014 Jun 12;123(24):3689-90. doi: 10.1182/blood-2014-03-563874. PMID: 24926069; PMCID: PMC4055918.
- Platt OS. Preventing stroke in sickle cell anemia. N Engl J Med. 2005 Dec 29;353(26):2743-5. doi: 10.1056/NEJMp058274. PMID: 16382060.
- Setty BN, Stuart MJ, Dampier C, Brodecki D, Allen JL. Hypoxaemia in sickle cell disease: biomarker modulation and relevance to pathophysiology. Lancet. 2003 Nov 1;362(9394):1450-5. doi: 10.1016/S0140-6736(03)14689-2. PMID: 14602439.
- Quinn CT, Variste J, Dowling MM. Haemoglobin oxygen saturation is a determinant of cerebral artery blood flow velocity in children with sickle cell anaemia. Br J Haematol. 2009 May;145(4):500-5. doi: 10.1111/j.1365-2141.2009.07652.x. Epub 2009 Mar 5. PMID: 19344400; PMCID: PMC2737449.
Figures:

Figure 1

Figure 2
Similar Articles
-
Congenital poisoning after maternal parenteral mercury administrationBenjamin Courchia*,Leventer Roberts Maya,Meyer John,Galvez Maida,Herrera Jaime,Rauch Daniel. Congenital poisoning after maternal parenteral mercury administration. . 2018 doi: 10.29328/journal.japch.1001001; 1: 001-005
-
The Impact of Adenotonsillectomy on Health-Related Quality of Life in Paediatric PatientsShuaib Kayode Aremu*. The Impact of Adenotonsillectomy on Health-Related Quality of Life in Paediatric Patients. . 2018 doi: 10.29328/journal.japch.1001002; 1: 006-011
-
Severe Infantile Transaldolase deficiency: A case reportKhaled Alqoaer*,Ziad Asaad,Maisa Halabi. Severe Infantile Transaldolase deficiency: A case report. . 2019 doi: 10.29328/journal.japch.1001003; 2: 001-003
-
Prevalence of ESBL urinary tract infection in childrenKhalil Salameh*,Galia ZA Awean,Hala Elmohamed,Hoor Alshmayt,Mohamed Riad Bur Omer . Prevalence of ESBL urinary tract infection in children. . 2019 doi: 10.29328/journal.japch.1001004; 2: 004-007
-
Does it matter what a mother consumes? An anthropological exploration of dietary practices among Churachandpur (Manipur) pregnant women and its impact on infant birth weightJS Sehrawat*,Evelyn Ngaithianven,Reetinder Kaur. Does it matter what a mother consumes? An anthropological exploration of dietary practices among Churachandpur (Manipur) pregnant women and its impact on infant birth weight. . 2019 doi: 10.29328/journal.japch.1001005; 2: 008-014
-
Glycemic status and its effect in Neonatal Sepsis - A prospective study in a Tertiary Care Hospital in NepalBadri Kumar Gupta*,Binod Kumar Gupta,Amit Kumar Shrivastava,Pradeep Chetri. Glycemic status and its effect in Neonatal Sepsis - A prospective study in a Tertiary Care Hospital in Nepal. . 2019 doi: 10.29328/journal.japch.1001006; 2: 015-019
-
Branchio Oculo Facial SyndromeMaha Oudrhiri*,Toualouth L,Houda Oubejja,Fouad Ettayebi,Hicham Zerhouni. Branchio Oculo Facial Syndrome. . 2019 doi: 10.29328/journal.japch.1001007; 2: 020-020
-
Current childhood cancer survivor long-term follow-up practices in South AfricaAnel van Zyl*,Mariana Kruger,Paul C Rogers. Current childhood cancer survivor long-term follow-up practices in South Africa. . 2020 doi: 10.29328/journal.japch.1001008; 3: 001-007
-
Aripiprazole-induced seizures in children with autism spectrum disorder and epilepsyMohammed MS Jan*. Aripiprazole-induced seizures in children with autism spectrum disorder and epilepsy. . 2020 doi: 10.29328/journal.japch.1001009; 3: 008-010
-
Case-based education to improve learning and faculty teaching of residents and students in a clinical settingDiane E Lorant*,Elizabeth A Wetzel. Case-based education to improve learning and faculty teaching of residents and students in a clinical setting. . 2020 doi: 10.29328/journal.japch.1001010; 3: 011-015
Recently Viewed
-
Obesity in Patients with Chronic Obstructive Pulmonary Disease as a Separate Clinical PhenotypeDaria A Prokonich*, Tatiana V Saprina, Ekaterina B Bukreeva. Obesity in Patients with Chronic Obstructive Pulmonary Disease as a Separate Clinical Phenotype. J Pulmonol Respir Res. 2024: doi: 10.29328/journal.jprr.1001060; 8: 053-055
-
Current Practices for Severe Alpha-1 Antitrypsin Deficiency Associated COPD and EmphysemaMJ Nicholson*, M Seigo. Current Practices for Severe Alpha-1 Antitrypsin Deficiency Associated COPD and Emphysema. J Pulmonol Respir Res. 2024: doi: 10.29328/journal.jprr.1001058; 8: 044-047
-
Navigating Neurodegenerative Disorders: A Comprehensive Review of Current and Emerging Therapies for Neurodegenerative DisordersShashikant Kharat*, Sanjana Mali*, Gayatri Korade, Rakhi Gaykar. Navigating Neurodegenerative Disorders: A Comprehensive Review of Current and Emerging Therapies for Neurodegenerative Disorders. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001095; 8: 033-046
-
Metastatic Brain Melanoma: A Rare Case with Review of LiteratureNeha Singh,Gaurav Raj,Akshay Kumar,Deepak Kumar Singh,Shivansh Dixit,Kaustubh Gupta*. Metastatic Brain Melanoma: A Rare Case with Review of Literature. J Radiol Oncol. 2025: doi: 10.29328/journal.jro.1001080; 9: 050-053
-
Validation of Prognostic Scores for Attempted Vaginal Delivery in Scar UterusMouiman Soukaina*,Mourran Oumaima,Etber Amina,Zeraidi Najia,Slaoui Aziz,Baydada Aziz. Validation of Prognostic Scores for Attempted Vaginal Delivery in Scar Uterus. Clin J Obstet Gynecol. 2025: doi: 10.29328/journal.cjog.1001185; 8: 023-029
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."