Abstract
Research Article
Comparison of Body Fat Percentage and BMI in Pre-hypertensive and Hypertensive Female College Students of West Tripura
Puja Saha, Satyapriya Roy, Susmita Banik, Sonali Das and Shilpi Saha*
Published: 03 April, 2025 | Volume 8 - Issue 1 | Pages: 001-006
Background: Obesity is a significant health risk linked to hypertension and heart-related disorders in adolescents, impacting their future well-being . Since, the present work is to determine the body constitute including percentage of body fat correlates with cholesterol level which associate with Body Mass Index.
Methods: This cross-sectional work was held in 120 college girls aged 19-23 years of Bhavan’s Tripura College of Science and Technology, Anandanagar at West Tripura. Anthropometric measurements such as standing height, body weight, sub scapular and triceps skinfolds, waist &hip circumference were collected. These records were used to calculate Body Fat Percentage (%BF) and Fat Mass (FM). Waist and Hip ratio (WHR) and Body Mass Index (BMI). FM, %BF and biochemical studies such as serum cholesterol level were also used to measures the body fat composition.
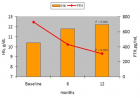
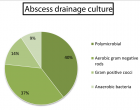
Results: According to the present study, 53.33% of girls have a normal BMI, 8.83% are underweight, 31.67% are overweight, and 6.67% are obese. WHR results indicate that 54.17% of participants are classified as obese and 45.83% as non-obese. Out of 114 (95%) girls with normal cholesterol levels of 16 (13.33%) students are pre-hypertensive and 10 (8.33%) students are hypertensive. Out of 38 overweight and 8 obese students 13.34% are in pre or hypertensive. Based on WHR, 65 (54.17%) female students are obese; out of 65 obese students, 12 (10%) and 7 (5.83%) female students are pre-hypertensive and hypertensive, respectively and this value is statistically significant (p value < 0.05). Out of 55 (45.83%) no-obese students 8 (6.67%) girls are pre-hypertensive and 5 (6.67%) girls are hypertensive. According to BMI female students who are overweight or obese (5%) also have excessive blood cholesterol.
Conclusion: This study expressed clear evidence of correlation in BMI, serum cholesterol level and Hypertension. These results are important for epidemiological studies to identify the cardiovascular risk in obese adults and help to solve a health problem of present Youngers in their future life. This study serves as an early health warning for female college students.
Read Full Article HTML DOI: 10.29328/journal.japch.1001070 Cite this Article Read Full Article PDF
Keywords:
BMI; Percent body fat; Obesity; Cardio vascular disease; Hypertension; Tripura
References
- Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, et al. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25-146. Available from: https://doi.org/10.1161/circulationaha.107.187998
- Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev. 2017;38(4):267-296. Available from: https://doi.org/10.1210/er.2017-00111
- Fruh SM. Obesity: risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 2017;29(SI):S3-S14. Available from: https://doi.org/10.1002/2327-6924.12510
- Kim H, Cho Y. Factors associated with metabolic syndrome among middle-aged women in their 50s: based on national health screening data. Int J Environ Res Public Health. 2020;17:3008. Available from: https://doi.org/10.3390/ijerph17093008
- Delgado A, Fernandez T, Martinez-Gonzalez M, Salas-Salvado J, Corella D, Castaner O, et al. The effect of physical activity and high body mass index on health-related quality of life in individuals with metabolic syndrome. Int J Environ Res Public Health. 2020;17:3728. Available from: https://doi.org/10.3390/ijerph17103728
- Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380:601-10. Available from: https://doi.org/10.1016/s0140-6736(12)60987-8
- Ungvari Z, Toth P, Tarantini S, Prodan CI, Sorond F, Merkely B, Csiszar A. Hypertension-induced cognitive impairment: from pathophysiology to public health. Nat Rev Nephrol. 2021;17:639-654. Available from: https://www.nature.com/articles/s41581-021-00430-6
- Williams B, Mancia G, Spiering W, Agabiti-Rosei E, Azizi M, Burnier M, et al. ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;36:1953-2041. Available from: https://doi.org/10.1093/eurheartj/ehy339
- World Health Organization. Hypertension [Internet]. Geneva: WHO; [accessed 2022 Dec 10]. Available from: https://www.who.int/news-room/fact-sheets/details/hypertension
- Centers for Disease Control and Prevention. Hypertension Cascade: Hypertension prevalence, treatment, and control estimates among U.S. adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2017-2020. Atlanta, GA: CDC; 2023 May 12 [accessed 2023 Jul 6].
- World Health Organization. World health statistics 2021: monitoring health for the SDGs, sustainable development goals. Geneva: WHO; 2021. License: CC BY-NC-SA 3.0 IGO. Available from: https://www.who.int/publications/i/item/9789240027053
- Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359-404. Available from: https://doi.org/10.1152/physrev.00033.2011
- Piche ME, Tchernof A, Despres JP. Obesity phenotypes, diabetes, and cardiovascular disease. Circ Res. 2020;126(11):1477-1500. Available from: https://doi.org/10.1161/circresaha.120.316101
- Despres JP. Body fat distribution and risk of cardiovascular disease. Circulation. 2012;126(10):1301-1313. Available from: https://doi.org/10.1161/circulationaha.111.067264
- Eveleth PB, Tanner JM. Worldwide variation of human growth. 2nd ed. Cambridge: Cambridge University Press; 1990.
- Reddon H, Gueant JL, Meyre D. The importance of gene-environment interactions of human obesity. Clin Sci. 2016;130:1571-97. Available from: https://doi.org/10.1042/cs20160221
- Shuster A, Patlas M, Pinthus JH, Mourtzakis M. The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br J Radiol. 2012;85(1009):1-10. Available from: https://doi.org/10.1259/bjr/38447238
- WHO Expert Consultation. Appropriate body-mass index in Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157-63. Available from: https://doi.org/10.1016/s0140-6736(03)15268-3
- Panagiotakos DB, Pitsavos C, Chrysohoou C, Risvas G, Kontogianni MD, Zampelas A, et al. The association between adherence to the Mediterranean diet and obesity status in the ATTICA study. Obes Res. 2004;12:1914-20.
- McGee BI, Diverse Population Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15:87-97. Available from: https://doi.org/10.1016/j.annepidem.2004.05.012
- Kragelund C, Hassager C, Hildebrandt P, Trop-Pedersen C, Kober L. Impact of obesity on long-term prognosis following acute myocardial infarction. Int J Cardiol. 2005;98:123-31. Available from: https://doi.org/10.1016/j.ijcard.2004.03.042
- Budimir D, Jeroneic A, Gunjaea G, Rudan I, Polasek O, Boban M. Sex-specific association of anthropometric measures of body composition with arterial stiffness in a healthy population. Med Sci Monit. 2012;18(2):Cr65-71. Available from: https://doi.org/10.12659/msm.882457
- Schorr M, Dichtel LE, Gerweek AV, Valera RD, Torriani M, Miller KK, et al. Sex differences in body composition and association with cardiometabolic risk. Biol Sex Differ. 2018;9(1):28. Available from: https://doi.org/10.1186/s13293-018-0189-3
- Wells JCK. The evolutionary biology of human body fatness: thrift and control. Cambridge: Cambridge University Press; 2010. Available from: https://doi.org/10.1017/CBO9780511691843
- Leung KC, Johannsson G, Leong GM, Ho KK. Estrogen regulation of growth hormone action. Endocr Rev. 2004;25:693-721. Available from: https://doi.org/10.1210/er.2003-0035
- Arakaki S, Maeshiro T, Hokama A, Hoshino K, Maruwaka S, Higashiarakawa M, et al. Factors associated with visceral fat accumulation in general population in Okinawa, Japan. World J Gastrointest Pharmacol Ther. 2016;7(2):261-267. Available from: https://doi.org/10.4292/wjgpt.v7.i2.261
- Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67(5):968-77. Available from: https://doi.org/10.1161/01.cir.67.5.968
- Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162(16):1867-72. Available from: https://doi.org/10.1001/archinte.162.16.1867
- Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566-75. Available from: https://doi.org/10.1001/archinternmed.2010.334
- Park SH, Choi SJ, Lee KS, Park HY. Waist circumference and waist-to-hip ratio as predictors of cardiovascular disease risk in Korean adults. Circ J. 2009;73(9):1643-50. Available from: https://doi.org/10.1253/circj.cj-09-0161
- Yamashita K, Kondo T, Osugi S, Shimokata K, Maeda K, Okumura N, et al. The significance of measuring body fat percentage determined by bioelectrical impedance analysis for detecting subjects with cardiovascular disease risk factors. Circ J. 2012;76(10):2435-42. Available from: https://doi.org/10.1253/circj.cj-12-0337
- Sandhu HS, Koley S, Sandhu KS. A study of correlation between lipid profile and BMI in patients with diabetes mellitus. J Hum Ecol. 2008;24(3):227-9. Available from: http://dx.doi.org/10.1080/09709274.2008.11906119
- Hussain S, Hussain I, Sana B, Waheed K, Qaisera S. Association of type 2 diabetes mellitus with biometric variables: a study in Sir Ganga Ram Hospital, Lahore. Ann King Edward Med Univ. 2009;15(2):48-53. Available from: https://doi.org/10.21649/akemu.v15i2.13
- Azizi F, Rahmani M, Emami H, Mimian P, Hajipur R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (Phase I). Soz Praventivmed. 2002;47(6):408-26. Available from: https://doi.org/10.1007/s000380200008
- Lee KS, Cho SD, Hong HS. The risk factors associated with increased blood pressure, sugar, and lipids in multiphasic health checkup examinees. Korean J Prev Med. 2000;33(2):69-75. Available from: https://www.jpmph.org/journal/view.php?number=204
- Lindsay RS, Hanson RL, Roumain S, Ravussin E, Knowler WC, Tataranni A. Body mass index as a measure of adiposity in children and adolescents: relationship to adiposity by dual-energy X-ray absorptiometry and to cardiovascular risk factors. J Clin Endocrinol Metab. 2001;86(9):4061-7. Available from: https://doi.org/10.1210/jcem.86.9.7760
- Costa GB, Horta N, Resende ZF, Souza G, Barreto LM, Correia LH, et al. Body mass index has a good correlation with pro-atherosclerotic profile in children and adolescents. Arq Bras Cardiol. 2009;93(3):261-7. Available from: https://doi.org/10.1590/s0066-782x2009000900010
- Aghasadeghi K, Zarei-Nezhad M, Keshavarzi A, Mehravani D. The prevalence of coronary risk factors in Iranian Lor migrating tribe. Arch Iran Med. 2008;11(3):322-5. Available from: https://pubmed.ncbi.nlm.nih.gov/18426325/
- Bakari AG, Onyemelukwe GC, Sani BG, Aliyu IS, Hassan SS, Aliyu TM. Relationship between random blood sugar and body mass index in an African population. Int J Diabetes Metab. 2006;14(4):144-5. Available from: http://dx.doi.org/10.1159/000497607
- Touitou Y, Portaluppi F, Smolensky MH, Rensing L. Ethical principles and standards for the conduct of human and animal biological rhythm research. Chronobiol Int. 2004;21(2):161-70. Available from: https://doi.org/10.1081/cbi-120030045
Figures:
Similar Articles
-
Effects of food programme for enhancing obesity children healthy of their abilities and expectations to self-efficacy for preventing early childhoodJirawon Tanwattanakul*,Suthiporn Sriprachote,Juraporn Tangpukdee,Nilawan Chanthapreeda,Toansakul Tony Santiboon. Effects of food programme for enhancing obesity children healthy of their abilities and expectations to self-efficacy for preventing early childhood. . 2021 doi: 10.29328/journal.japch.1001040; 4: 093-100
-
Obesity and Sex as Determinants of Atherogenic Risk Associated with High-Density (HDL) and Low-Density Lipoprotein (LDL) Subfractions in Adolescents: A Population-based Study Based on Health Survey of Sao PauloMarlene N Aldin, Regina M Fisberg, Marcelo M Rogero, Flavia M Sarti, Nágila RT Damasceno*. Obesity and Sex as Determinants of Atherogenic Risk Associated with High-Density (HDL) and Low-Density Lipoprotein (LDL) Subfractions in Adolescents: A Population-based Study Based on Health Survey of Sao Paulo. . 2024 doi: 10.29328/journal.japch.1001068; 7: 052-061
-
Comparison of Body Fat Percentage and BMI in Pre-hypertensive and Hypertensive Female College Students of West TripuraPuja Saha,Satyapriya Roy,Susmita Banik,Sonali Das,Shilpi Saha*. Comparison of Body Fat Percentage and BMI in Pre-hypertensive and Hypertensive Female College Students of West Tripura. . 2025 doi: 10.29328/journal.japch.1001070; 8: 001-006
Recently Viewed
-
Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting ChildrenErwin Gunawan*,Ria Puspitawati. Relationship between Vitamin D Deficiency and Lipopolysaccharides Porphyromonas gingivalis Bacteria in Stunting Children. Ann Biomed Sci Eng. 2024: doi: 10.29328/journal.abse.1001033; 8: 059-065
-
Addiction to self-strangulation: a case-reportAurely Ameller*,Yann Le Strat,Marion Cadranel,Celine Portalier, Caroline Dubertret. Addiction to self-strangulation: a case-report . J Addict Ther Res. 2017: doi: 10.29328/journal.jatr.1001003; 1: 016-021
-
Nanoencapsulated Extracts from Leaves of Bauhinia forficata Link: In vitro Antioxidant, Toxicogenetic, and Hypoglycemic Activity Effects in Streptozotocin-induced Diabetic MiceBárbara Verônica Cardoso de Souza, Alessandra Braga Ribeiro*, Rita de Cássia Meneses Oliveira, Julianne Viana Freire Portela, Ana Amélia de Carvalho Melo Cavalcante, Esmeralda Maria Lustosa Barros, Luís Felipe Lima Matos, Tarsia Giabardo Alves, Maria. Nanoencapsulated Extracts from Leaves of Bauhinia forficata Link: In vitro Antioxidant, Toxicogenetic, and Hypoglycemic Activity Effects in Streptozotocin-induced Diabetic Mice. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001063; 8: 100-115
-
Oral Suspension as Versatile Galenic Formulation in PediatryMauro Luisetto*, Almukthar N, Edbey K, Mashori GR, Fiazza C, Dona’ l, Cabianca L, Latyshev O. Oral Suspension as Versatile Galenic Formulation in Pediatry. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001062; 8: 091-099
-
Modulation of Microbiota and its Impact on DepressionKousik Maparu*. Modulation of Microbiota and its Impact on Depression. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001061; 8: 089-090
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."