More Information
Submitted: 23 November 2020 | Approved: 07 December 2020 | Published: 08 December 2020
How to cite this article: Jansen L, Colleran G, Okafor I, Quinn N. A rare case of acute necrotising pancreatitis in a paediatric patient. J Adv Pediatr Child Health. 2020; 3: 061-063.
DOI: 10.29328/journal.japch.1001020
Copyright License: © 2020 Jansen L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Child presenting with acute abdominal pain
A rare case of acute necrotising pancreatitis in a paediatric patient
Lizeri Jansen1*, Gabrielle Colleran2, Ikechukwu Okafor1 and Nuala Quinn1
1Department of Paediatric Emergency Medicine, Children’s Health Ireland at Temple Street, Dublin, Ireland
2Department of Radiology, Children’s Health Ireland at Temple Street, Dublin, Ireland
*Address for Correspondence: Lizeri Jansen, Department of Paediatric Emergency Medicine, Children’s Health Ireland at Temple Street, Dublin, Ireland, Tel: +353 83 396 5133; Email: [email protected]
The diagnosis of acute necrotising pancreatitis is a rare event in the Paediatric Emergency Department (ED).
We report a case of acute pancreatitis in a paediatric patient, diagnosed in our ED, a tertiary level paediatric hospital.
This child presented with vague symptoms of constipation, abdominal pain and back pain, and on clinical examination had a distended abdomen with peritonism. She rapidly deteriorated and needed aggressive fluid resuscitation in the ED for treatment of septic shock. The diagnosis of acute pancreatitis (AP) was only considered once elevated amylase levels were apparent.
Whilst AP is an important differential diagnosis in a patient who is presenting with acute abdominal symptoms, the diagnosis in children in particular is seldom and thus easily overlooked in the previously healthy child.
The incidence of acute pancreatitis (AP) is estimated 3.6-13.2 per 100 000 children per year. It is therefore an important differential for children with an acute abdominal presentation, however the cases are few [1]. Paediatric cases are estimated to be <1% of all cases of acute necrotizing pancreatitis [2].
The possible causes of AP in the paediatric population include infections (eg mumps, measles, salmonella), drugs (salicylic acid, valproic acid, steroids, alcohol), trauma, systemic disease (eg autoimmune disorders like systemic lupus erythematosus), metabolic disorders (eg hyperlipoproteinaemia, diabetes, hypercalcaemia), and anatomic anomalies (eg choledochal cyst). Sometimes the cause is idiopathic [3-5].
Diagnosis is made by the symptoms (usually vomiting and abdominal pain) [6], pancreatic lipase and amylase levels and imaging [7,8]. Imaging may show pleural effusion, ileus, a sentinel loop sign or colon cut-off sign [9,10]. Ultrasound is a useful non-invasive modality to assess the pancreas, but CT scanning is superior for early diagnosis especially when ultrasound findings are non-specific [11,12]. MRCP is essential in patients where no cause is found, as this may show underlying anatomic anomalies [13].
An 8 year old girl presented to our emergency department (ED) by ambulance with reported vague symptoms of constipation for one week. For the past 3 days, she had worsening central abdominal pain, back pain and dysuria. There was no reported nausea or vomiting. Her parents were concerned that she appeared lethargic on that day. She had no fever, no sick contacts and no recent trauma. According to her mother, the patient passed a small amount of hard stool that morning after a microlax enema.
No comorbidities were known and there was no family history of significance. Of note in her history, she had a previous laparoscopic appendectomy in 2019 after presenting with severe abdominal pain and vomiting for 1 day. The appendix histology showed a normal appendix, her mother remembers she was unwell after the procedure and needed 6 days of intravenous antibiotics for fever and a high CRP. The cause for her unusual symptoms were attributed to a possible mesenteric adenitis.
On physical examination, there was abdominal distension and resonance to percussion. The patient was tachycardic (130 bpm) and pale, however able to mobilize around the department. She started vomiting shortly after her arrival to the ED. Upon second review (one hour after first assessment) she had further deteriorated, with worsening abdominal pain, hypertension (131/61 mmHg) and sudden severe pallor.
The abdominal examination had changed: she became peritonitic, with guarding and rebound tenderness. Point of Care Ultrasound (POCUS) Echocardiography revealed a hyperdynamic left ventricle consistent with sepsis. The inferior vena cave was collapsed, supporting a diagnosis of septic shock [14].
The differential diagnosis at this point expanded to include bowel obstruction, malrotation and bowel perforation.
The patient was resusciated with two intravenous (IV) fluid boluses of 20 ml/kg 0.9% saline. Fluid resusication was guided by POCUS echocardiography. IV broad spectrum antibiotics (cefotaxime and gentamicin) were administered. Fluid resusciation improved the patient’s haemodynamics – pulse rate settled between 80 and 90 bpm. Given the severity of the patient’s abdominal pain, ketamine boluses were administered with excellent analgesic effect.
Supine abdominal x-ray showed prominent gas-filled bowel loops, with no fluid levels and a paucity of gas in the rectum. Chest x-ray showed no significant findings and importantly, no pneumoperitoneum. An abdominal ultrasound was performed which demonstrated multiple dilated loops of bowel, areas of free fluid in the abdomen and generalized hyperechogenicity of the mesentery.
Blood results showed CRP 270 mg/L; amylase 1951 U/L. It was only with the amylase result that AP was considered.
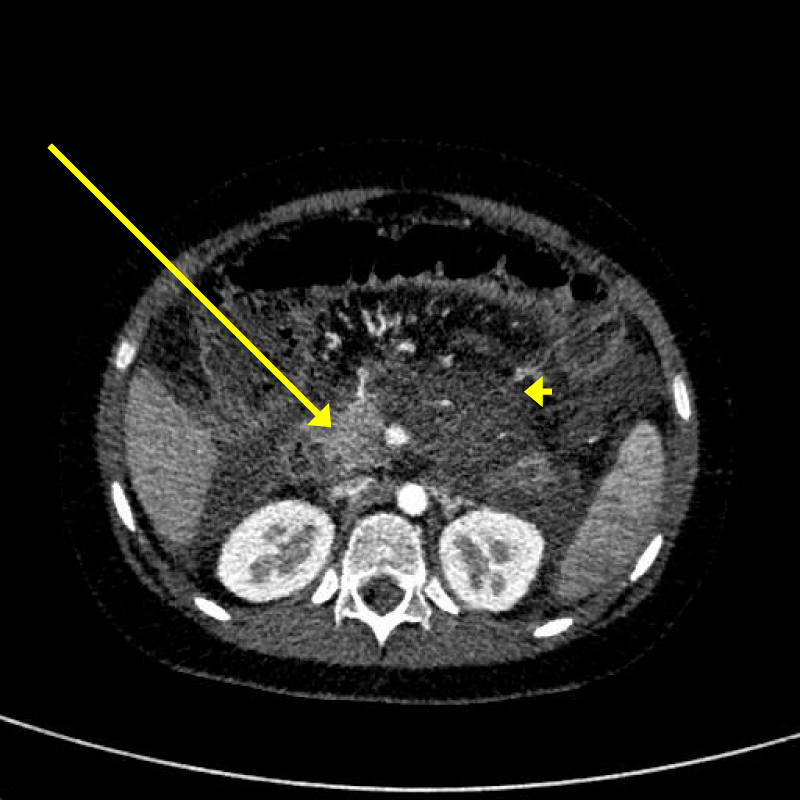
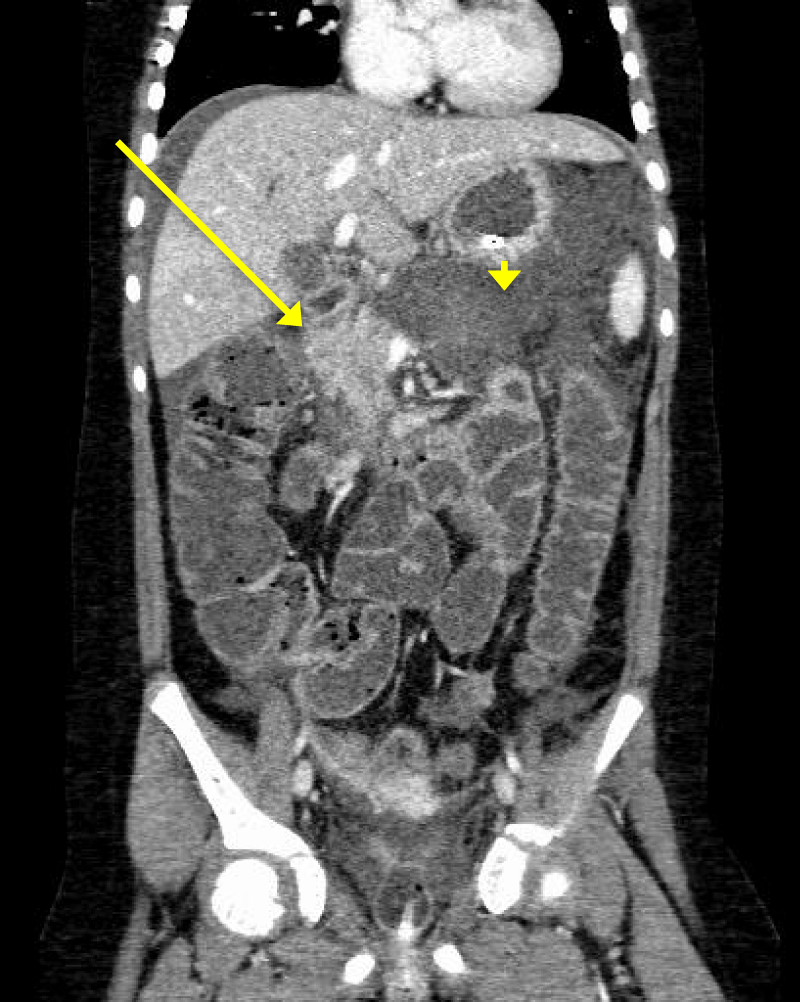
CT abdomen demonstrated features consistent with severe acute necrotic pancreatitis with acute necrotic collection (Figures 1,2). There was also a filling defect at the splenic vein suggestive of splenic vein thrombosis. There was no possible underlying aetiology identified: there was distension of the gallbladder and intrahepatic biliary dilatation, possibly attributed to reactive oedema of the pancreatic head. There was no evidence of bowel obstruction. There were bilateral pleural effusions with left sided lung atelectasis.
Figure 1: Axial contrast enhanced abdominal CT at the level of the pancreas. The head is enhancing normally (yellow arrow). Abnormal low attenuation and swelling is seen of the body of the pancreas (yellow arrowhead).
Figure 2: Coronal contrast enhanced abdominal CT at the level of the pancreas. The head is enhancing normally (yellow arrow). Abnormal low attenuation and swelling is seen of the body of the pancreas (yellow arrowhead). Free fluid is seen adjacent to the right lobe of the liver below the diaphragm.
She was admitted to the paediatric ward for supportive care, however the following day became tachypnoeic, hypoxic, tachycardic and developed a fluid imbalance requiring admission to our intensive care unit (ICU). A COVID screen was performed and yielded a negative result. There was initial slow improvement to high flow nasal cannula oxygenation and total parenteral nutrition via nasojejunal feeds. Her fluid retention required 6 days of furosemide. On the recommendation of a paediatric haematologist, she was administered a low molecular weight heparin (Tinazeparin) for splenic vein thrombosis. This was stopped due to worsening lower abdominal and flank bruising and abnormal coagulation profile, which was corrected with vitamin K administration. The patient developed hyperglycaemia and was administered novorapid as needed. IV Piperacillin Tazobactam was commenced and after 4 days she was fit for discharge from ICU. After a 4 week inpatient stay, she was finally discharged home.
A cause for the netrotising pancreatitis has not yet been found and she is undergoing detailed medical assessment.
Children with AP most often presents with abdominal pain and vomiting. Diagnosis is made with elevated serum amylase and confirmatory imaging (Ultrasound and CT abdomen). There are many causes for AP in children, and often, the underlying diagnosis is never found.
There is a vast list of aetiologies of AP in the paediatric population. After trauma, the most common causes includes systemic disease, drugs, infections, metabolic disorders and anatomic anomalies like a choledochal cyst. Systemic disease includes autoimmune causes such as systemic lupus erythematosus, inflammatory bowel disease and henoch-schonlein purpura. Drugs that commonly cause AP are salicylic acid, valproic acid, steroids and alcohol. Infections include mumps, measles, Epstein-Barr virus and salmonella. Metabolic disorders that have been associated with AP include hypercalcaemia, alpha-1 antitrypsin deficiency, diabetes mellitus and hyperlipiaemia. Often, the cause is deemed idiopathic after all the above causes have been excluded [3].
Abdominal pain and to a lesser extent distension, are very common presentations to the Paediatric ED. Our patient presented with these common symptoms. She acutely deteriorated in our ED, with signs of sepsis and peritonitis, but the diagnosis of pancreatitis, given its rarity, was not initially considered until an elevated serum amylase was evident. Acute deterioration may require extensive resuscitation in order to minimise complications and improve patient outcome.
AP should be an important differential in a child presenting with acute abdominal pain, and it mimics many disease processes. Although acute necrotizing pancreatitis is a rare finding, it can cause significant morbidity and a high index of suspicion should be maintained when approaching these cases. Timely, effective resucitation in the ED is of the utmost importance.
- Valabrega S, Bersigotti L, Antolino L, Aurello P, Tomassini F, et al. Pediatric Pancreatitis: Not a Rare Entity, Pancreatitis, Dmitry Victorovich Garbuzenko. IntechOpen. 2019. https://www.intechopen.com/books/pancreatitis/pediatric-pancreatitis-not-a-rare-entity
- Whitcomb DC, Lowe ME. Pancreatitis: Acute and chronic. In: Kleinman RE, Sanderson IR, Goulet O, et al., editors. Walker’s Pediatric gastrointestinal disease. Hamilton: BC Decker Inc; 2008; 1213–1220.
- Nydegger Couper RT, Oliver MR. Childhood pancreatitis. J Gastroenterol Hepatol. 2006; 21: 499–509. PubMed: https://pubmed.ncbi.nlm.nih.gov/16638090/
- Benifla M, Weizman Z. Acute pancreatitis in childhood: analysis of literature data. J Clin Gastroenterol. 2003; 37: 169–172. PubMed: https://pubmed.ncbi.nlm.nih.gov/12869890/
- Werlin SL, Kugathasan S, Frautschy BC. Pancreatitis in children. J Pediatr Gastroenterol Nutr. 2003; 37: 591–595. PubMed: https://pubmed.ncbi.nlm.nih.gov/14581803/
- Ziegler DW, Long JA, Philippart AI, Klein MD. Pancreatitis in childhood. Experience with 49 patients. Ann Surg. 1988; 207: 257–261. PubMed: https://pubmed.ncbi.nlm.nih.gov/3345113/
- Agarwal N, Pitchumoni CS, Sivaprasad AV. Evaluating tests for acute pancreatitis. Am J Gastroenterol. 1990; 85: 356–366. PubMed: https://pubmed.ncbi.nlm.nih.gov/2183590/
- Abu-El-Haija M, Kumar S, Quiros JA, Balakrishnan K, Barth B, et al. Management of Acute Pancreatitis in the Pediatric Population: A Clinical Report From the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition Pancreas Committee. J Pediatr Gastroenterol Nutr. 2018; 66: 159-176. PubMed: https://pubmed.ncbi.nlm.nih.gov/29280782/
- Stein GN, Kalser MH, Sarian NN, Finkelstein A. An evaluation of the roentgen changes in acute pancreatitis: correlation with clinical findings. Gastroenterology. 1959; 36: 354–361. https://pubmed.ncbi.nlm.nih.gov/13640153/
- Pickhardt PJ. The colon cutoff sign. Radiology. 2000; 215: 387–389. PubMed: https://pubmed.ncbi.nlm.nih.gov/10796912/
- Silverstein W, Isikoff MB, Hill MC, Barkin J. Diagnostic imaging of acute pancreatitis: prospective study using CT and sonography. AJR Am J Roentgenol. 1981; 137: 497–502. PubMed: https://pubmed.ncbi.nlm.nih.gov/7025598/
- Lautz TB, Turkel G, Radhakrishnan J, Wyers M, Chin AC. Utility of the computed tomography severity index (Balthazar score) in children with acute pancreatitis. J Pediatr Surg. 2012; 47: 1185–1191. PubMed: https://pubmed.ncbi.nlm.nih.gov/22703791/
- Shimizu T, Suzuki R, Yamashiro Y, Segawa O, Yamataka A, et al. Magnetic resonance cholangiopancreatography in assessing the cause of acute pancreatitis in children. Pancreas. 2001; 22: 196–199. PubMed: https://pubmed.ncbi.nlm.nih.gov/11249076/
- Alonso JV, Turpie J, Farhad I, Ruffino G. Protocols for Point-of-Care-Ultrasound (POCUS) in a Patient with Sepsis; An Algorithmic Approach. Bull Emerg Trauma. 2019; 7: 67-71. PubMed: https://pubmed.ncbi.nlm.nih.gov/30719469/